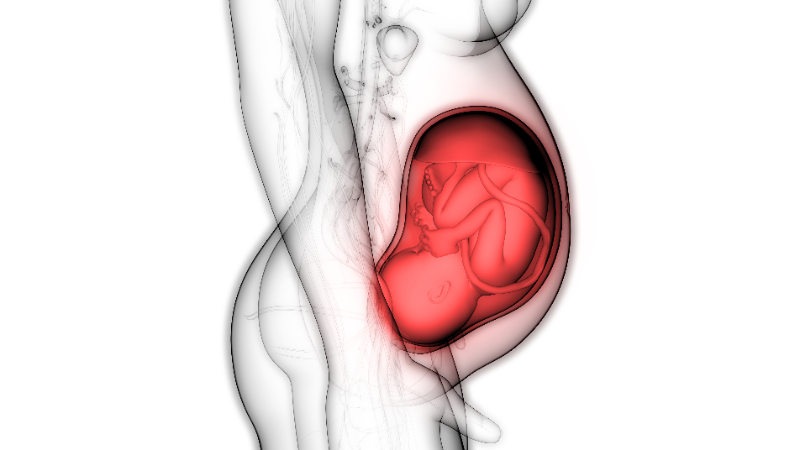
While many expectant moms have visions of cradling their newborn baby, they also think of possible complications. As your baby’s due date draws closer, what should you know about a possible complication known as umbilical cord prolapse (UCP)? This means the cord comes out before the baby does and could get severely compressed – cutting off blood vital nutrients and oxygen flow to the fetus.
When my very pregnant friend was told to see a specialist right away, she brushed it off. But when her OB/GYN made an appointment on her behalf, she took heed. It turned out that the umbilical cord was severely constricted – and she was placed in the hospital immediately. This article describes causes, risks and techniques for handling UCP. Empower yourself by knowing what can be done about it to help your baby.
What Is Umbilical Cord Prolapse?
When the cord falls (prolapses) through the cervix and into your vagina before the baby passes through, it means the baby’s head is not engaged in your pelvis as it should be. So, the cord could get trapped against the baby’s body. However, UCP has happened much less often (only 1 in 300 births) in recent years, thanks to progress made in managing it.
Causes: Why Does it Happen?
Most cases of cord prolapse are due to risks that could not be prevented. These can include:
- Abnormal presentation of the baby
- Prematurity
- Uterine irregularities
Less than half of the cases of UCP occurred due to obstetric intervention – an action done with the intention to help the birth mom; yet, it had a negative result. Such an intervention could be from an attending provider or could occur during a diagnostic procedure or medical treatment. UCP might happen after interventions like fetal blood sampling or artificial rupture of the membranes (also called amniotomy).
Although such interventions can be responsible in some cases of cord prolapse, other major causes of UCP include:
- Premature rupture of membranes (occurring naturally). The sudden change in pressure pushes the baby down toward the cervix relatively fast. This becomes an emergency because any part of the baby could press on the cord, cutting off the baby’s oxygen source.
- Prolonged decrease in heart rate. If your baby has a continuous decline in heart rate, this could mean that there is constant pressure on the cord. Your provider could view this on the fetal monitor or in a cervical exam.
- Delivery of more than one baby. If you are having multiple babies, then the baby that comes out first might push out the cord.
- Excess amniotic fluid. If there is too much fluid, the pressure might push the umbilical cord out.
- Breech baby. If your baby’s position is breech (feet down), then this could make enough space for the cord to slide through the birth canal first. In one study, breech presentation accounted for 36.5% of UCP cases.2
- Hyperactivity of the baby. There are rare occasions when the baby is hyperactive while you’re pregnant. This could also cause cord compression.
A woman may have a higher risk of UCP if she:
- is greater than or equal to 35 years of age
- is pregnant with multiple babies
- gave birth to other children in the past
- has a baby with a low birth weight
- had preterm labor (less than 37 weeks)

What Can be Done to Help the Baby?
Once it has been determined that there is UCP, then the provider has about 30 minutes from diagnosis to treatment.
- Cesarean section is the preferred method for delivering the baby if UCP occurs. That being said, deliveries by C-section have been associated with a greater risk of fetal injuries than vaginal delivery (18.5% vs 8.7%). Keep in mind, however, that cesarean delivery is "significantly associated with decreased perinatal mortality and morbidity compared to vaginal delivery," according to a study published in the American Journal of Obstetrics and Gynecology.1 The researchers found that delivery by emergency C-section significantly reduced the risks of neonatal death compared with a normal vaginal delivery.
- Vaginal delivery may be considered, especially in the second stage of labor – and if it is considered "feasible, quick, and highly likely to succeed."
- Measures to relieve the cord compression are usually tried – if the method to resolve this complication is expected to take too long. The following might be attempted:
- Rotate the baby's head if he/she is in an abnormal position.
- Press on or raise the baby's presenting body part – to take pressure off the cord
- Place an intrauterine pressure catheter
- Vago's method (bladder filling)
- Put the mom's head lower than her pelvic region
More techniques for preventing cord prolapse:
- Awareness and anticipation of the risk factors
- Antenatal ultrasound diagnosis in high risk patients
- Vigilance during procedures that increase the risk of UCP, such as
- Amniotomy
- Manual rotation of the head
- Application of cervical ripening balloon and fetal scalp electrodes
It is difficult to eliminate the risk of UCP completely with these strategies. But, being prepared for this complication could lead to earlier diagnosis and intervention – and best of all, better outcome.
What is The Risk of Fatality?
The risk of death of the baby from UCP is about 10%. Much of this risk is due to premature birth or congenital anomalies. The reason a premature baby has a higher rate of cord prolapse is because it has a smaller volume filling the pelvis along with a relative increase in the volume of fluid around it.
Deaths associated with UCP have gone down, thanks to better neonatal care and obstetric management. Indeed, infant mortality has declined from 375 per 1,000 to approx. 36 and 162 per thousand live births in the last century.
Umbilical cord prolapse (UCP) is an uncommon but potentially fatal obstetric emergency. Its incidence has fallen over the years and advances in managing UCP have led to better outcomes.
